26M with fever, vomitings and loose stools
History of presenting illness
Patient was apparently asymptomatic 12 days ago, then, he developed fever which was high grade, intermittent, associated with chills and rigor.
He developed vomitings 9 days ago, 5 episodes, with food as content, non bilious, non projectile, non blood stained
Loose stools 9 days ago, 3 episodes/day, watery, green coloured, not blood stained.
H/o green coloured stools since 9 days.He apparently drank papaya leaf juice for 3days in the morning prior to the episodes of loose stools.
He also had headache and generalised weakness since 12 days
He visited a doctor but symptoms still persisted so he came to our hospital on 7/6/23
Past history
Not a k/c/o DM, HTN, Tuberculosis,epilepsy, asthma.
No H/o similar complaints in the past
Personal history
Appetite-Normal
Diet-mixed
Bowel movements- increased
Sleep-Adequate
Addictions- Has been drinking alcohol (375ml) everyday since 6 years
Family history
Insignificant
Treatment history
Paracetamol and sporlac
General examination
Patient is conscious, coherent and cooperative; well oriented to time,place and person
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, pedal edema
Vitals
Temp- 99.8°F
PR- 84 bpm
RR- 16 cpm
BP- 100/70mmHg
Systemic examination
GIT
Inspection-
Shape of the abdomen- Scaphoid
Umblicus- inverted
No scar,pigmentation, engorged veins ,peristaltic waves.
Hernial orifices are normal.
All quadrants move equally with respiration
Palpation
No local rise in temperature
Liver span- 14cm
Consistency-soft,non tender
Surface-smooth
Margins-rounded
Percussion
Tympanic resonance heard.
Auscultation
Gurgling bowel sounds heard.
RS-B/L air entry present
Normal vesicular breath sounds heard
CVS- S1S2 present, no murmurs heard
Investigations
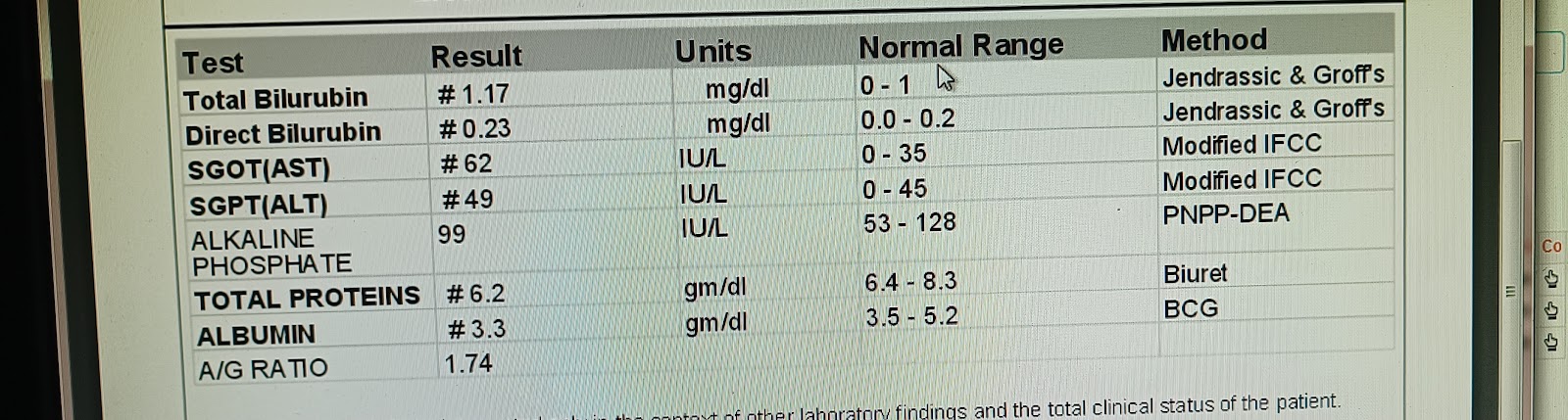
Liver function tests
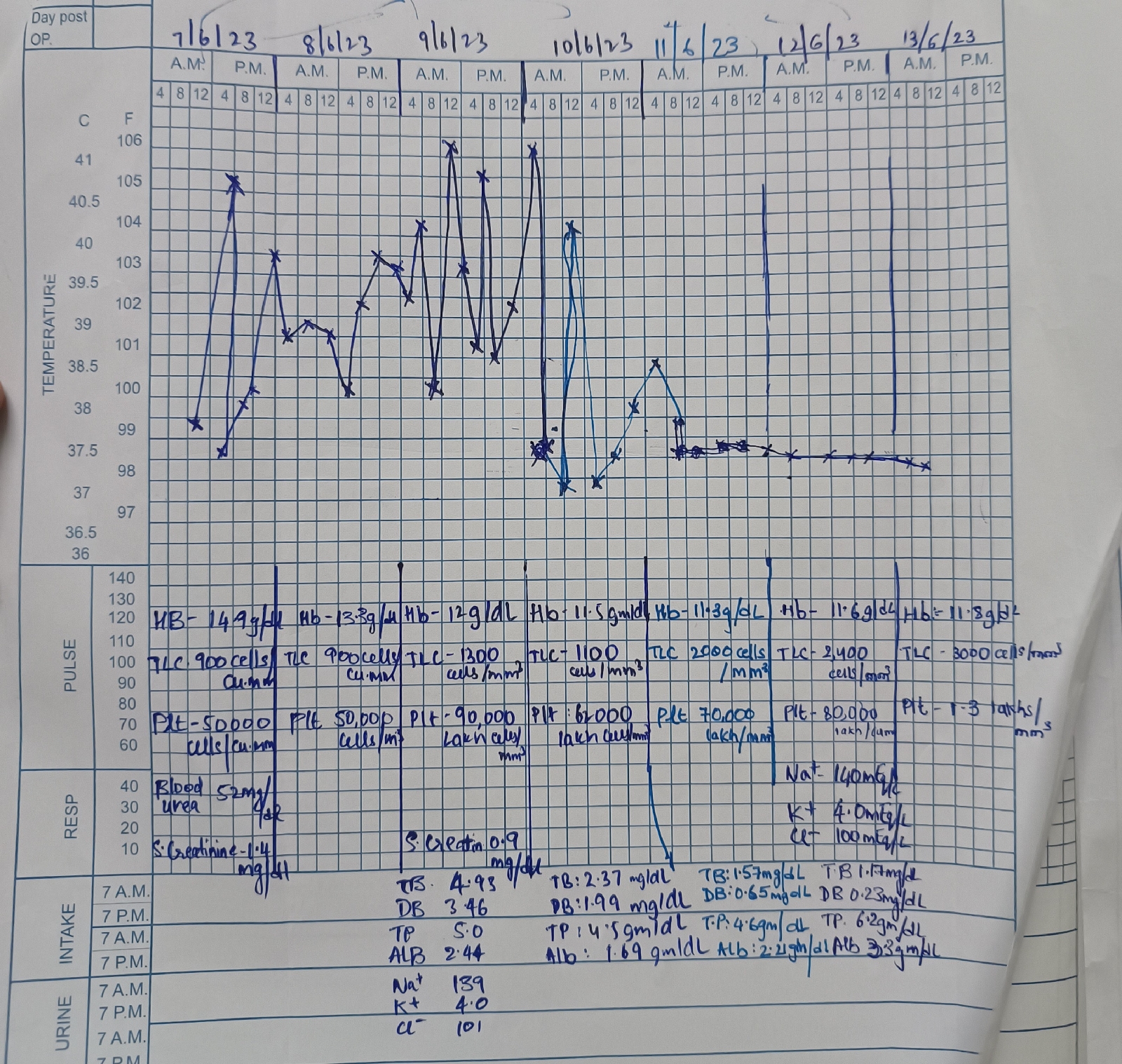
Haemogram
Fever chart
Pyrexia w/ pancytopenia and hepatomegaly
?Malaria
Treatment:
1.IV FLUIDS NS, DNS, RL@ 50 ml/hr
2. Inj. Doxycycline 100mg IV/BD
3. Plenty of oral fluids
4.Protein rich diet
5.Monitor vitals



Comments
Post a Comment